HINWEIS: Dieses Produkt und seine Zubehörteile sind nicht für die Verwendung innerhalb der EU und des Vereinigten Königreichs bestimmt. Bitte wenden Sie sich an das Vertriebsteam, um Informationen über nichtmedizinische Alternativprodukte zu erhalten.
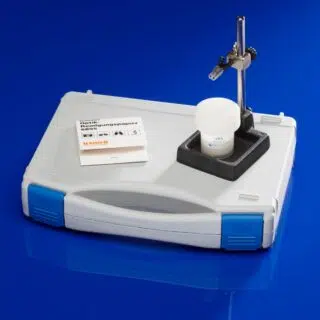
Der moorVMS-LDF Laser-Doppler Blutfluss- und Temperaturmonitor ist ein medizintechnisches Hochleistungsgerät sowohl für den klinischen Einsatz als auch für den Laborgebrauch. Durch den Einsatz moderner Mikroprozessortechnolgie ist es uns gelungen, Ihnen ein leichtes und portables Gerät zu einem unschlagbaren Preis anbieten zu können, ohne dabei Abstriche bei den Spezifikationen, der Qualität oder der Zuverlässigkeit machen zu müssen.
Für noch anspruchsvollere Forschungsvorhaben können Sie mit der Software moorVMS-PC auch Blutdruck-, Iontophorese- und Hauterwärmungsmodule sowie den Oxygenierungsmonitor moorVMS-OXY simultan in Ihre Versuchprotokolle einbinden. Mit dem neuen moorVMS-DAQ können Sie zudem acht weitere externe Signalquellen erfassen. Sie zudem weitere externe Signalquellen erfassen. Unsere Software bietet Ihnen zudem eine Reihe von automatischen Standardauswertungen und natürlich die Möglichkeit, die Analysen Ihren Bedürfnissen anzupassen.
Das moorVMS-LDF bietet Ihnen:
- Ein- und Zweikanaloption
- Vielkanaloption: Kombinieren Sie unsere Module zu einem Vielkanalsystem, das Sie mit unserer Software nach Ihren Wünschen konfigurieren. Dank unseres modularen Designs können Sie alle Geräte aufeinander stellen. Dies spart Platz in Ihrem Setup!
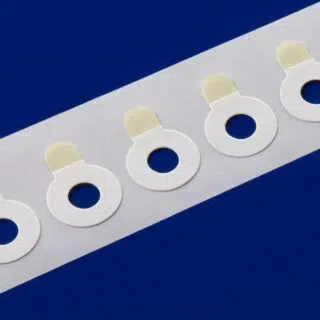
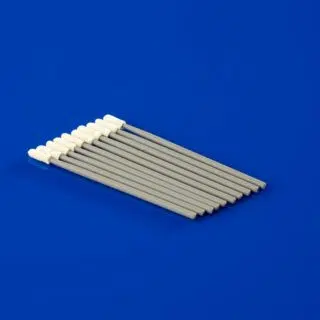
- Unsere „MemoryChip-Sensoren“ gibt es für eine Vielzahl von Anwendungen. Die aktuellen Kalibrierungsdaten sind im Sensor selbst gespeichert. Ein Software-Assistent erinnert Sie an eine eventuell notwendige Neukalibrierung. Alle unsere Hautsensoren haben einen eingebauten Temperatursensor
- Gute Lesbarkeit durch ein hintergrundbeleuchtetes weißes Hochkontrast-LCD
- Fortschrittliche Windows™ kompatible moorVMS-PC Software mit umfangreichen Analysefunktionen und automatischer Reportgenerierung. Mehr Informationen zu Softwarefunktionen finden Sie in den moorVMS-LDF links
- Einfach zu verbinden: Als Standard stehen Ihnen der analoge Ausgang (0-5 Volt, BNC) und der digitale USB-Port zum Übertragen der Daten in Echtzeit zu Verfügung
- Das medizintechnische Design erlaubt die Anwendung sowohl in der Klinik als auch in der Forschung
- Die mehrsprachige DVD können Sie als ständige Referenz nutzen
- Garantierte Zuverlässigkeit: 5 Jahre Herstellergarantie.